Submitted by kmcochran on

Based on the demonstration of outstanding Quality Improvement Methodology PQCNC is proud to announce Novant Health as the recipient of the 2021 PQCNC Quality Award for their project Reduction of Primary Cesarean (RPC).
The PQCNC Quality Improvement Award recognizes a North Carolina unit that has made a measurable and sustained positive change in a major perinatal quality improvement indicator/issue through the implementation of quality improvement activities within the previous three years. Projects are reviewed for design, team development, adherence to QI principles, documentation and reporting of PDSAs, identifying clear aims for the project, tracking and reacting to key process and outcome measures designed to achieve initiative aim.
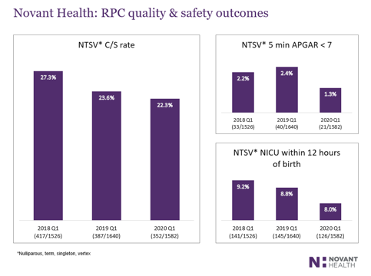
This years winner organized a team with members from 8 North Carolina and 2 Virginia birthing facilities and had a goal of standardizing low-risk maternity care across our healthcare system by targeting the reduction of primary C-section. Notably, reducing primary C-section rates below 23.9% develop the opportunity to: 1) improve the quality of care in our communities, on current and subsequent pregnancies, while impacting care in the future 2) address care inequities across populations and 3) significantly impact the unsustainable financial burden of healthcare in our country.
In the course of exceeding their target the multidisciplinary team identified challenges, opportunities and implemented changes in practice including:
- A pre-cesarean checklist,initially piloted at Novant Health Presbyterian Medical Center (PMC) and later introduced at all obstetric (OB) hospitals across the organization
- Guidelines for clinical milestones, that support failure to progress or failed induction of labor diagnoses, have been integrated into practice
- Monthly reports identifying NTSV C-section patients with documented indications of labor dystocia while not satisfying the 15 hour guideline of rupture of membranes (ROM) with Pitocin augmentation prior to posting
- QI teams engage in peer reviews of these variances and communicate findings to leadership
- Tracking balancing measures to ensure patient safety
Resulting in:
- The ability to track structural, process, and outcome measures for all NTSV deliveries across multiple facilities in a complex healthcare setting, establishing a framework for success
- Reinforcement of best practice, through the adoption of a pre-cesarean checklist, promoted optimal care provision and standardized management of the NTSV labor process
- Transparency related to provider performance facilitated meaningful discussions that fostered engagement and generated momentum
Congratulations to the team for your inspiring work and your commitment to making North Carolina the best place to give birth and be born!

