For those of you requiring IRB approval - click here
Joining the Initiative
Please submit a PQIT Roster for your team
Please complete the Phase II Snapshot for your facility
Initiative Data:
The official start date for initiative data is March 1 2015. Any patient admitted on March 1 that is scored is eligible for the NAS database.
Charter
Action Plan
Data collection form
Data dictionary
Accessing reports
Data Submission: Please do not complete and hold forms, but instead enter data regularly into Delphi so that our work and our reports will be current - daily entry is best!
Attention Data Collectors: click here for instructions of how to obtain access to Delphi to submit data.
PDSA:
Please chose one area for improvement from the action plan and begin your work. Complete the PDSA worksheet and return by March 1st 2015.
Roster Changes: Please make sure to send me any changes in your team roster. We would like to be able to provide all team members with the latest information about the initiative and we can only do that with your help.
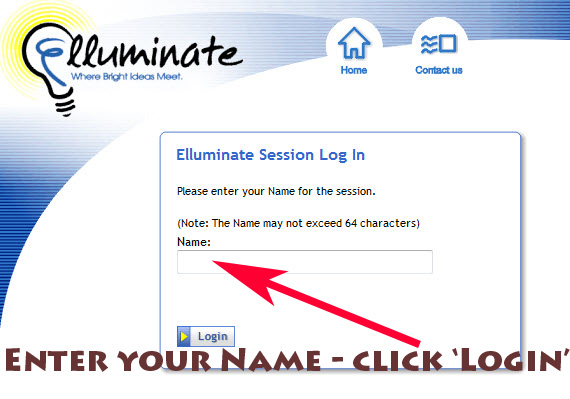
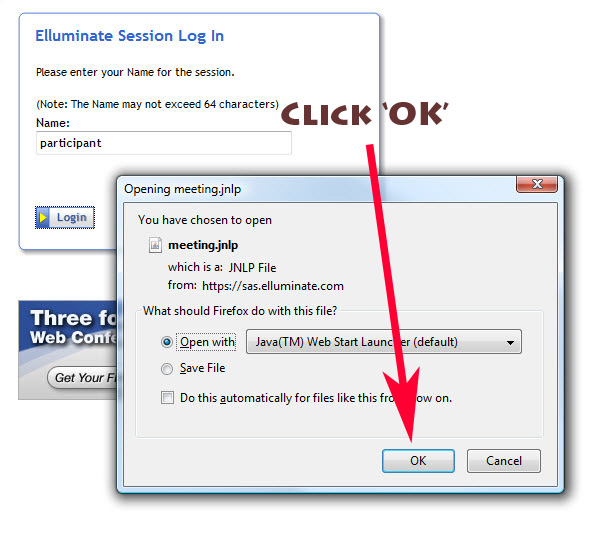
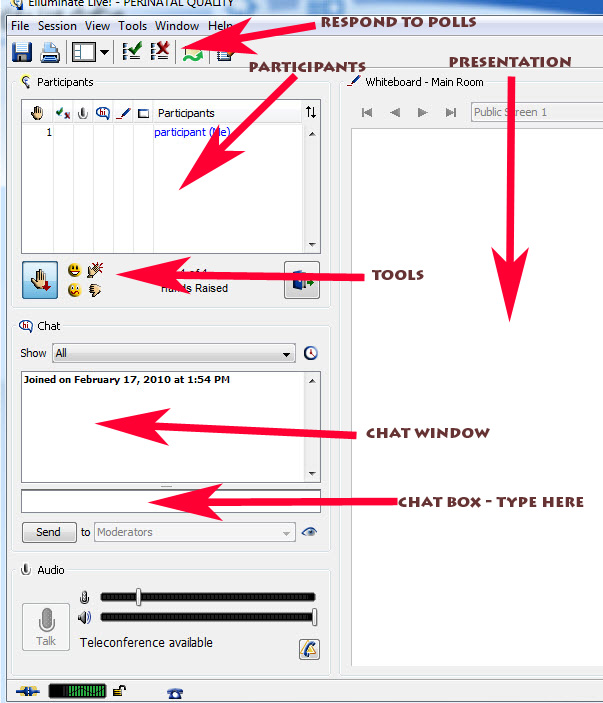
Webinars: Monthly webinars will be held on the 2nd Tuesday of every month at 12:00pm beginning Tuesday January 13th. Please go ahead and reserve these dates on your calendars. Your team will need to schedule at least monthly meetings to review data, make plans for PDSA cycles, and plan for next steps. Please set up times to meet with your Executive Champions to update them on your progress and to ask for their help to meet your goals. PQCNC would suggest you meet with them every other month but no less than every quarter.