Labor support education has been an emphasis for all teams working to reduce primary cesarean deliveries. Many facilities had labor support classes scheduled that were cancelled due to COVID and are working to have that education rescheduled. One resource for labor support that can be readily available are doulas. Frye Regional Medical center is utilizing a local doula, Laura Nance, to provide staff education on labor support. Laura is a senior advisor at the Childbirth and Postpartum Professional Association (CAPPA) and has a wealth of experience and knowledge to share with obstetric staff. With many hospitals banning employee travel and conferences due to COVID, utilizing a local resource to continue to improve practice and reduce cesarean deliveries is pure genius!
Updates
Labor support education has been an emphasis for all teams working to reduce primary cesarean deliveries. Many facilities had labor support classes scheduled that were cancelled due to COVID and are working to have that education rescheduled. One resource for labor support that can be readily available are doulas. Frye Regional Medical center is utilizing a local doula, Laura Nance, to provide staff education on labor support. Laura is a senior advisor at the Childbirth and Postpartum Professional Association (CAPPA) and has a wealth of experience and knowledge to share with obstetric staff. With many hospitals banning employee travel and conferences due to COVID, utilizing a local resource to continue to improve practice and reduce cesarean deliveries is pure genius!
Many of the facilities working to increase labor support education to laboring women and staff have utilized printouts of laboring positions that are readily available in the labor room. A staff nurse at UNC has taken that education a step further. Kara Robinson, RN, recognized a need for patients at UNC to have education about labor provided in various formats. Kara partnered with a UNC nurse educator, Danielle Anspach, to create a powerpoint presentation depicting positions for all stages of labor. Kara recruited nurse and ancillary staff at UNC to portray laboring women and demonstrate proper positioning in photographs that also included a written description of each position. Soothing background music was then added to wrap up the presentation. The presentation was added to UNCs patient education television curriculum, is available at all times and is being translated in Spanish. This is a tremendous resource for women delivering at UNC! Congratulations to Kara, Danielle, and the UNC team in their effort to make North Carolina the best place to give birth and be born!
Congratulations to several outstanding hospitals in North Carolina for being recognized in Newsweek as the Best Maternity Hospitals of 2020! Newsweek magazine partnered with The Leapfrog Group to recognize hospitals for excellence in maternity care considering factors such as cesarean section rates, episiotomy rates, early elective deliveries and protocols in place to protect mothers and babies.
- Alamance Regional Medical Center
- Atrium Health Cleveland
- Duke Regional Hospital
- Duke University Hospital
- Harris Regional Hospital
- Maria Parham Hospital
- McDowell Hospital
- New Hanover Regional Medical Center
- Novant Brunswick
- Novant Huntersville
- Novant Matthews
- Novant Presbyterian
- Novant Thomasville
- Randolph Health
- Sentara Albemarle Hospital
- University of North Carolina
- Wake Forest Baptist - Lexington
- Wake Med Raleigh
Vidant Health is working to bring ongoing fetal monitoring education to all of its birthing facilities. Jennifer Kendrick, the Perinatal Outreach Coordinator and an AWHONN Fetal Monitoring Instructor for Vidant Health, provides email education each month to all labor and delivery staff and providers throughout the Vidant system. Jennifer identifies strips to target specific educational needs, such as tachysystole, abruption and fetal distress, and emails a sample strip along with a case study and a series of questions regarding interpretation and subsequent interventions. When responses are submitted, Jennifer provides corrective guidance as appropriate. Fantastic work by Jennifer and the Vidant system in keeping fetal monitoring education in the forefront of care delivery!
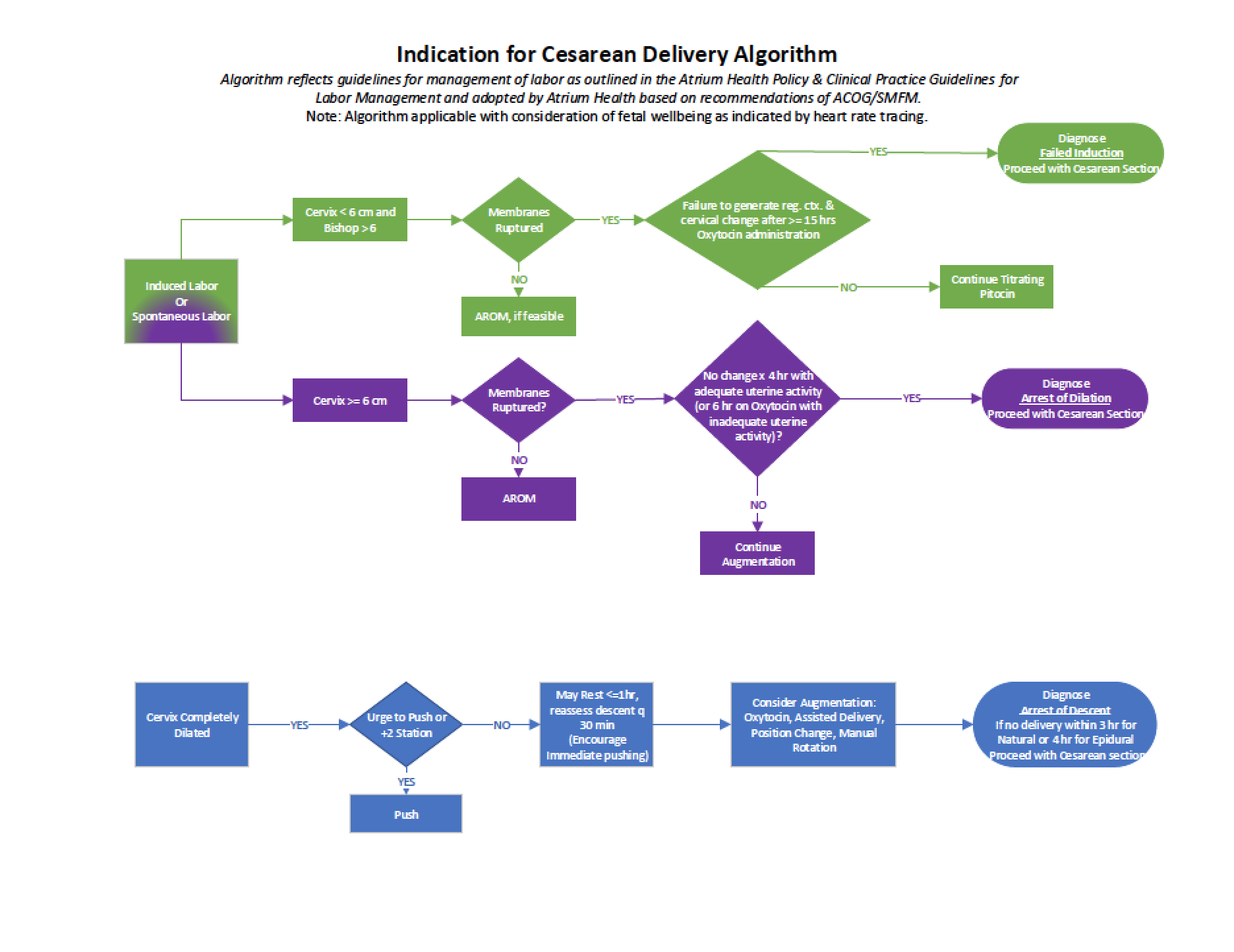
Mission hospital was one of the first PQCNC RPC teams to create a labor algorithm utilizing the criteria found in the ACOG/SMFM CS checklist. Their algorithm was color coded and easy to follow. Through the course of the RPC initiative, Atrium Health built off of Mission’s work and added further detail to their labor algorithm. Atrium Health vetted the algorithm through staff and providers and the final version went live in May 2020. These algorithms are wonderful visual tools to guide decision making in supporting laboring women.
After the last RPC learning session in March 2020 focused on improving knowledge around fetal monitoring, several teams moved to implement different approaches to reviewing monitoring strips with staff and providers. A few teams have begun to review sample fetal monitoring strips at staff meetings while other teams are reviewing strips at shift huddles. The strip review, followed by a brief discussion of the interpretation and interventions to follow, works to ensure that all staff are utilizing appropriate terminology and provides for sharing of ideas about effective ways to respond. Additionally. discussions around appropriate documentation of interventions, both of content and location in the EMR, are important in capturing care provided.
On March 3, 2020 RPC teams gathered face to face for the day to collaborate and brainstorm on how to continue making great strides toward our goal of an overall statewide NTSV cesarean rate of 20% by January 2021. Since the focus over the past year has largely been on following ACOG criteria for failed induction and labor dystocia, the content of the learning session centered on the clinical indication of fetal concern and the impact fetal heart rate (FHR) interpretation has on the decision to perform a surgical birth. Presenters discussed unique educational sessions created for both providers and nurses focused on fetal heart rate interpretation. The sessions were successful in large part due to the short duration of the class to easily fit the busy schedule of obstetricians. Additionally, the unique perspective from a legal nurse expert was part of the discussion as she shared how to minimize risk as a labor nurse when documenting and responding to electronic fetal heart rate tracings. Lastly, large group discussions ensued at the end of the day as actual fetal heart rate strips were shared and interpreted along with resuscitative actions that should follow.
The next learning session for the PQCNC AIM RPC initiative is scheduled for March 3, 2020. Presentations will be offered by several of our wise peers who have honed their craft over time. Chris Westveer, a clinical nurse specialist from Atrium Cabarrus, will be sharing a fetal monitoring update class for providers, Mona Ketner, a legal nurse consultant and nurse educator from Northwest AHEC, will share some legal insights on fetal monitoring and Heather Talley, the Nurse Manager of Labor and Delivery at Duke Regional, will discuss how she has crafted a high level of collaboration between physicians, midwives and nurses to produce outstanding patient outcomes. Dr. Ollendorff will be reviewing RPC data to date and guiding us through the nuances of interpreting and responding to fetal monitoring strips. A day full of collaboration of sharing of wisdom from those who have experienced success.
In order to increase shared decision making between mothers and the medical team, one hospital is extending childbirth education to provider offices. Frieda Norris at CaroMont created a brief class titled “Preparing for Vaginal Birth” that is advertised and conducted at provider offices twice a month. The class gives information for women to consider when preparing for birth and encourages them to register for the more detailed childbirth education classes at CaroMont. Frieda is the friendly face that teaches class at the provider offices and also teaches childbirth education at CaroMont so parents have a familiar contact when attending classes.
