Teams from across the state gathered for our face to face learning session this month to celebrate gains and focus on sustaining their improvements. Our keynote speaker, Dr. Bryan Sexton, Associate Professor in Psychiatry and Behavioral Sciences at Duke University School of Medicine, presented his work on avoiding burnout and enhancing resiliency in healthcare workers. Perinatal Quality Improvement Teams (PQITs) spent much of the day developing their next rapid-cycle improvement plan with the intention of achieving 100% on time to treatment and control and patient education over the final four months of the initiative.
Updates
Teams have been working to implement their projects related to transforming the patient care experience, but the work doesn’t end there… Teams are focusing on the importance of ongoing monitoring of projects and the sharing of results. Monitoring projects in a structured, thoughtful way allows teams to quickly identify challenges and continually celebrate successes - this is especially important as teams focus on small tests of change. To help facilitate the sharing of results, teams were provided with customizable report templates to assist them with summarizing their work and capturing the most important data.
An important aspect of the CMOP initiative is to not only educate patients but engage and empower them in their care. Teams took education a step further and measured their patient’s knowledge around the signs and symptoms of postpartum preeclampsia that warrant prompt treatment after discharge.
With a focus on teach-back responses, PQCNC designed an informational tool that explained three questions to ask patients before discharge, answers to listen for, and what to do if they respond incompletely. Using this tool and the PQCNC designed tracking tool, teams were able to measure the effectiveness of their education practices. If patients are unable to answer the questions on the informational tool staff are instructed to re-educate and seek out additional resources to provide follow-up support.
These efforts are aimed at ensuring no mother will go home without knowing her risk and what to do to avoid potentially fatal complications related to postpartum preeclampsia.
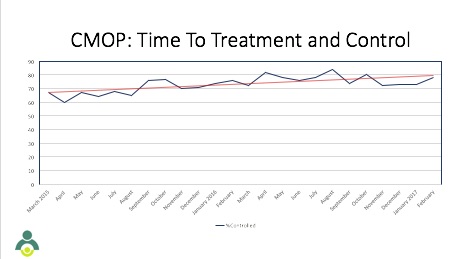
CMOP teams are in the final year of the initiative and have started out the year continuing to improve upon the work they have already accomplished. A constant focus during the initiative has been monitoring time to treatment and control for hypertensive patients and CMOP teams have demonstrated continual improvement in efficiently managing hypertension.
Over the next several months, CMOP teams will be examining methods to sustain their improvement efforts ensuring progress continues.
Our CMOP teams have spent the past several months improving the care and outcomes of their patients and their infants by focusing on administering a full course of antenatal steroids on those at risk for pre-term delivery.
As outlined in the ACOG guidelines, treatment with corticosteroids is recommended for pregnant women between 24 and 34 weeks of gestation and is associated with significant reductions in neonatal morbidity and mortality.
Our teams completed small tests of change to ensure all staff were educated on the critical timing of optimal administration of corticosteroids. Additionally, teams focused on standardizing care across the state from large tertiary centers to small referral centers.
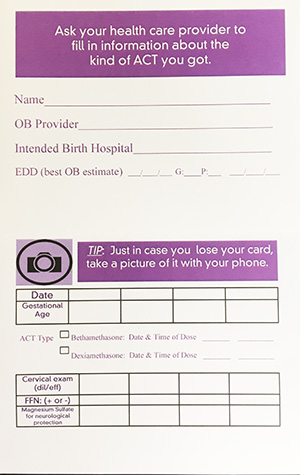
As with all our initiatives at PQCNC, we recognize the success we achieve would be suboptimal without the partnership and collaboration of our patients and families. Implementation of an Antenatal Steroid (ANS) Passport tool that incorporates the patient in care, was one of our most successful achievements in meeting our goal of full course steroid administration. This tool ensures the patient is at the center of her care and provides a means to facilitate communication between doctors and facilities.
If an at-risk mother enters a triage or small referral center and receives a dose of steroids, she is given a passport tool which documents necessary details of the steroid she receives. She is encouraged to carry this card with her, as well as take a photo of it with her phone, in order to provide accurate medical information to the next hospital or doctor she visits.
Incorporating patients in their care is a simple and necessary to achieve optimal outcomes in this special population and at times complicated system of care.
Intentional partnering with patients and their families is the foundation for achieving optimal clinical outcomes and successful quality improvement initiatives. The CMOP action plan outlines goals and change ideas to assist teams in ensuring that patients and their families are partners both at the organizational level and at the bedside. In our August webinar, three of our PQIT teams shared stories outlining the clinical progress that has resulted in their units as a result of partnering with patients. Each presentation reflected a different level of engagement and presented evidence on how each patient’s role in that partnership differed – allowing teams to identify a path that could fit with the culture of their own units.
Moving forward teams will, in partnership with patients and families, conduct a formal assessment of their patient- and family-centered care practices and use their localized findings to drive their efforts and allow for a more personalized focus on patient activation – ensuring our perinatal patients are empowered and have the information and tools they need to become actively engaged in their care.
2016 has proven to be a successful one for CMOP PQITs. There were three measures that demonstrated success from January through April 2016. Those three measures include time to treatment and control and decreasing deliveries prior to 37 weeks for gestational hypertension and mild preeclampsia.
Time to Treatment and Control averaged just above 75%, which is the highest percentage of controlled patients in a consecutive four month time period since the initiation of CMOP. 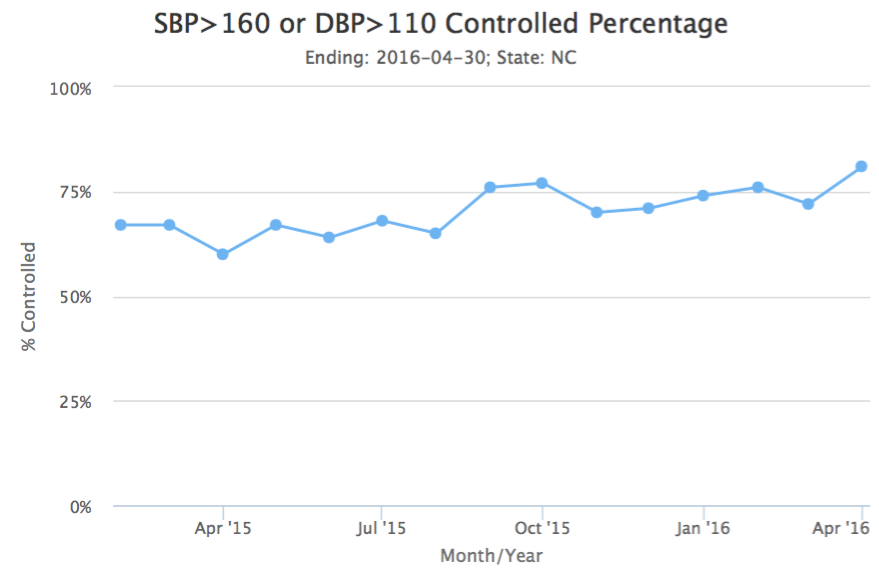
In the same consecutive four month time frame, early deliveries indicated by a diagnosis of gestational hypertension decreased to 61 and early deliveries by a diagnosis of mild preeclampsia were even lower at 36.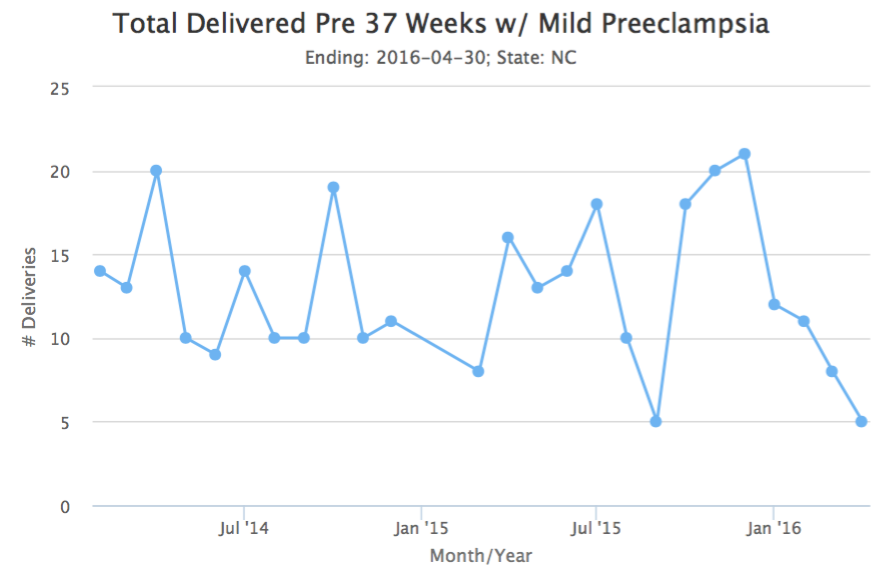

While there continues to be opportunities for improvement, the work done by PQITs is having a positive impact on expectant mothers and babies in NC moving us closer to the goal of being the best place to give birth and be born.
Magnesium sulfate has been used in obstetrics for decades to protect both moms and babies. Articles were shared with the CMOP teams to encourage reflection of their own hospital protocols regarding magnesium administration. Suggestions outlined in these articles encouraged the use of ACOG’s Patient Safety Checklist focused on magnesium sulfate administration in anticipated pre-term deliveries to provide neuroprotection for the infant. Additionally, the research highlights the benefit of administering magnesium to pre-eclamptic mothers for seizure control.
Antenatal corticosteroids (ANS) have been shown to reduce the risk of serious health problems and death among preterm infants - evidence suggests that ANS administration rates can and should be optimized to reach more than 90% of eligible pregnant women as a way to improve outcomes for babies born too soon.
Our current focus is to ensure pregnant women between 24 weeks and 34 weeks of gestation who are at risk of preterm delivery within 7 days, receive a full course of corticosteroid treatment. Teams will concentrate their efforts on developing guidelines for proper and timely administration of ANS and will devise PDSAs aimed at improving the patients understanding of why ANS treatment is beneficial and essential to the outcome of their baby.
Teams are wrapping up their 4 month intensive on bedside engagement in preparation for the next Learning Session which will be on May 17 at the McKimmon Center in Raleigh. The intensive work by teams resulted in new ways of engaging and teaching patients, new resources developed and implemented, and a steadily increasing rate of successful 'teach back', our proxy measure for engagement. At the upcoming Learning Session, Perinatal Quality Improvement Teams (PQITs) will wrap up their intensive focus on engagement by learning how to use TeamSTEPPS strategies for engaging patients and families at the bedside. The next steps in the CMOP Action Plan will be reviewed and teams will begin an intensive focus on antenatal steroid use and magnesium administration. Tracy Manuck, MD, MS will be kicking off the discussion by highlighting the benefits and issues surrounding antenatal steroid administration. Tracy is the Assistant Director of the Prematurity Prevention Clinic at UNC and practices Maternal Fetal Medicine. Margarita Bidegain, MD, MHS-CL, Associate Professor of Pediatrics at Duke, is co-leading this phase for PQCNC and will be addressing the PQITs on the state of antenatal steroid use in North Carolina.
