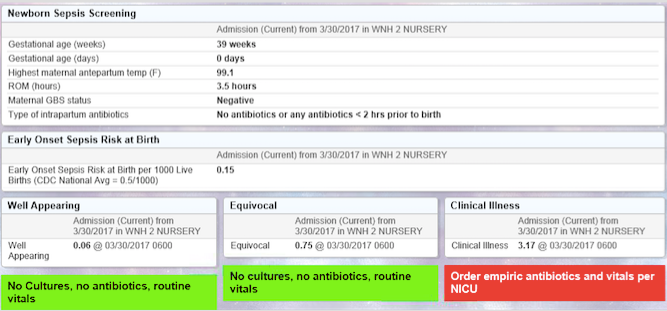
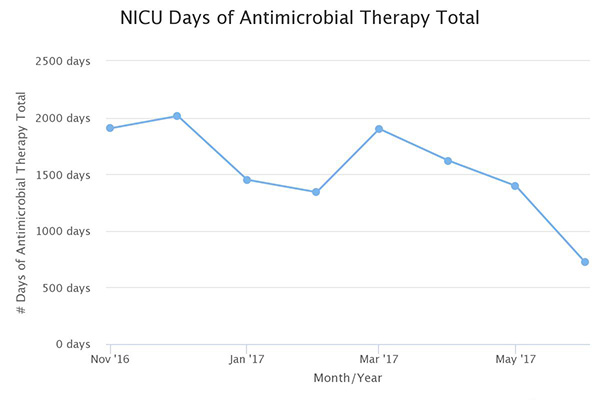
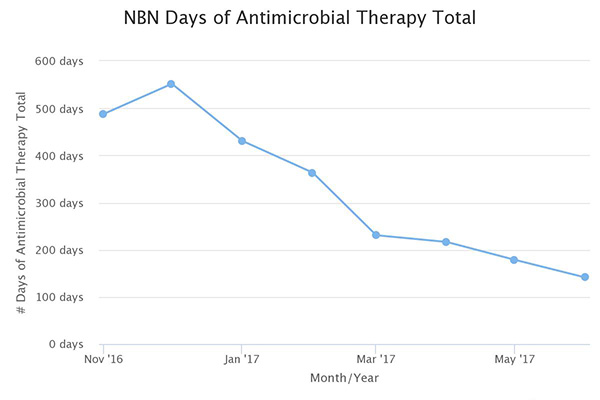
Over the past 12 months, nurseries reduced antibiotic exposure by 50% saving exposure for over 1100 infants. However, the most profound outcome of the initiative was the collaboration our teams experienced demonstrating once again that state collaboratives are THE venue for rapid high impact quality improvement work. Neonatologist were engaged and eager to learn from Pediatricians and many times it was the nursery leading the way for the NICU. The catalyst of integrating the sepsis calculator on infants in newborn nurseries spread such practices as defining at-risk guidelines for all infants, adopting a 36 hour stop time if cultures were negative, and adapting sepsis order sets to include treatment by doses versus treatment length that varied by provider. Some teams even replaced their current GBS order sets with the Kaiser sepsis calculator, integrated the risk score in their EMR and created sustainable, system changes that will impact all newborns greater than 34 weeks, long after this initiative comes to a close.
These accomplishments were not easy but all ASNS teams were successful as a result of their dedication to improve care, willingness to share lessons learned and most importantly, collaborate across unit lines.