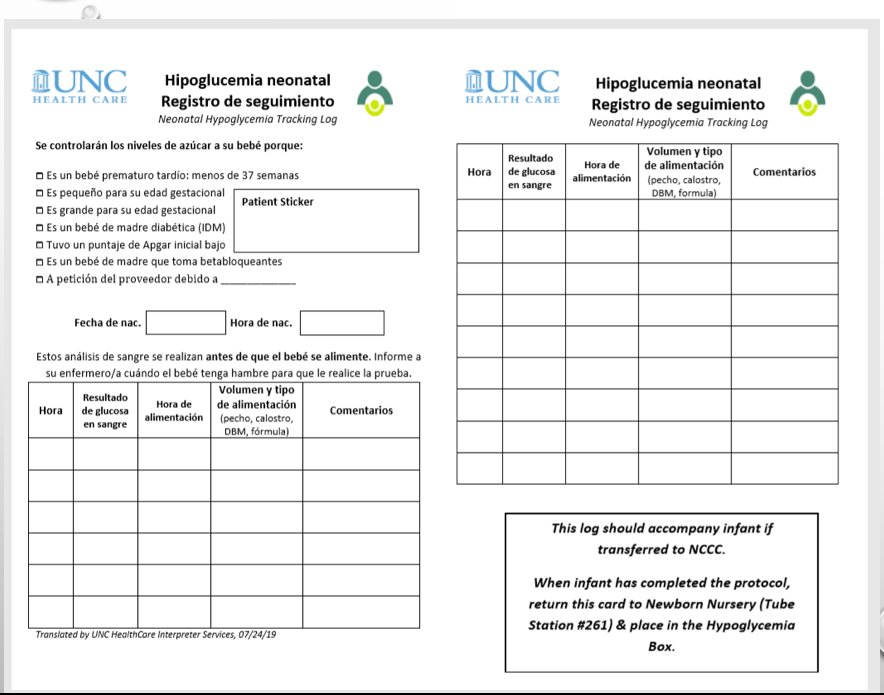
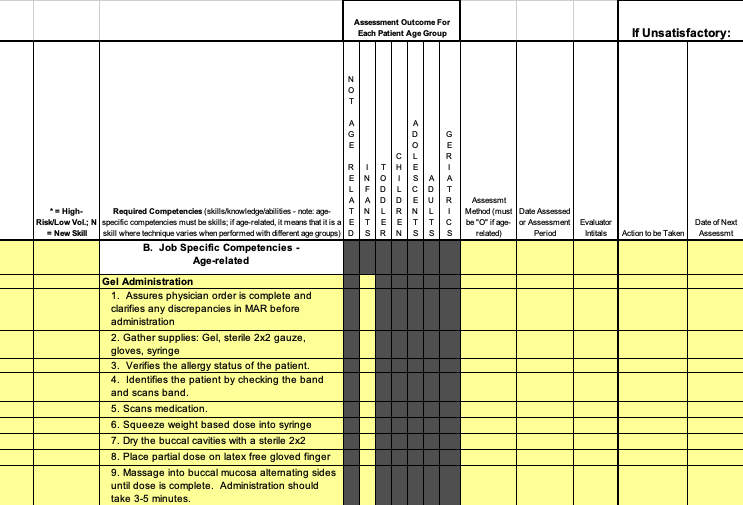
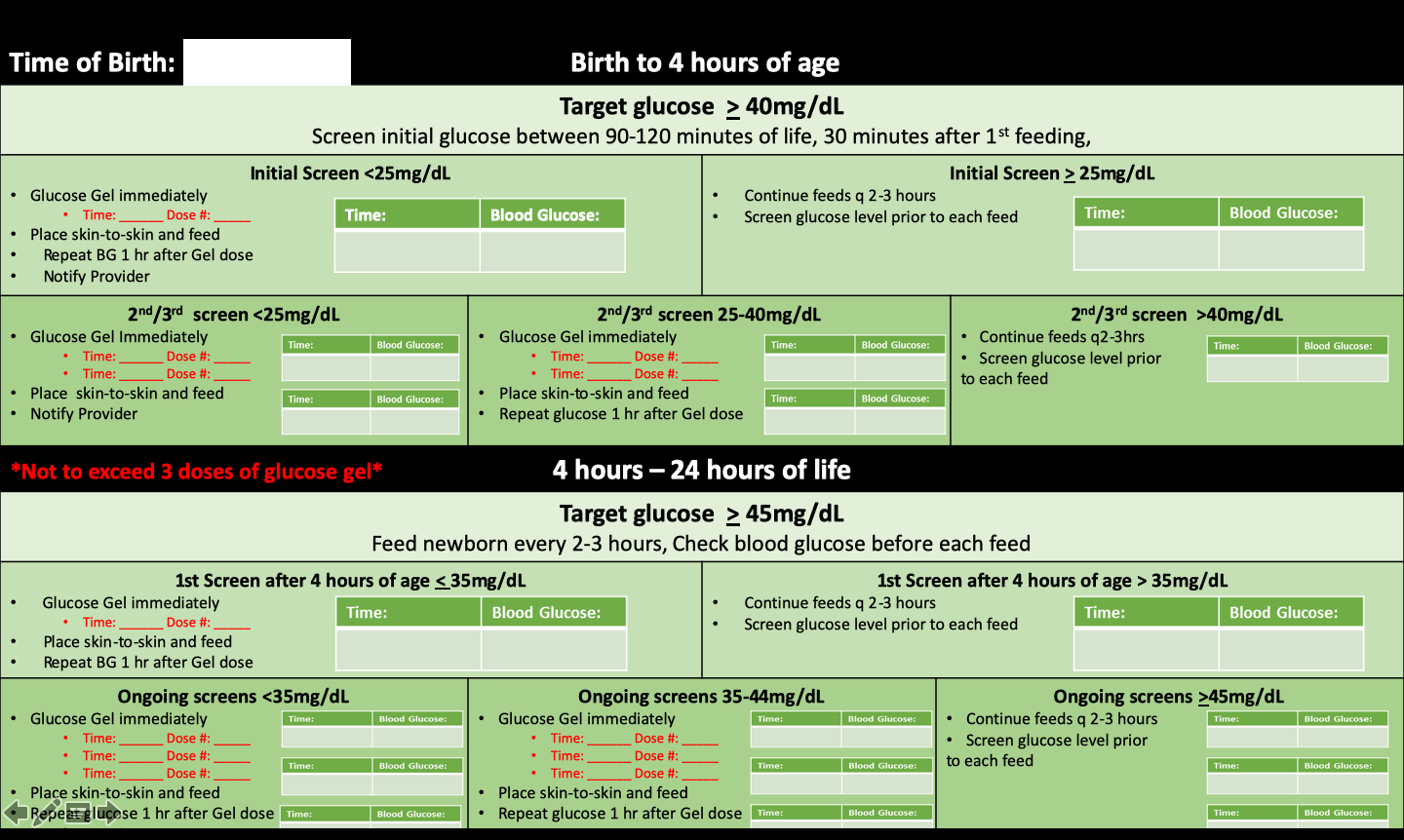
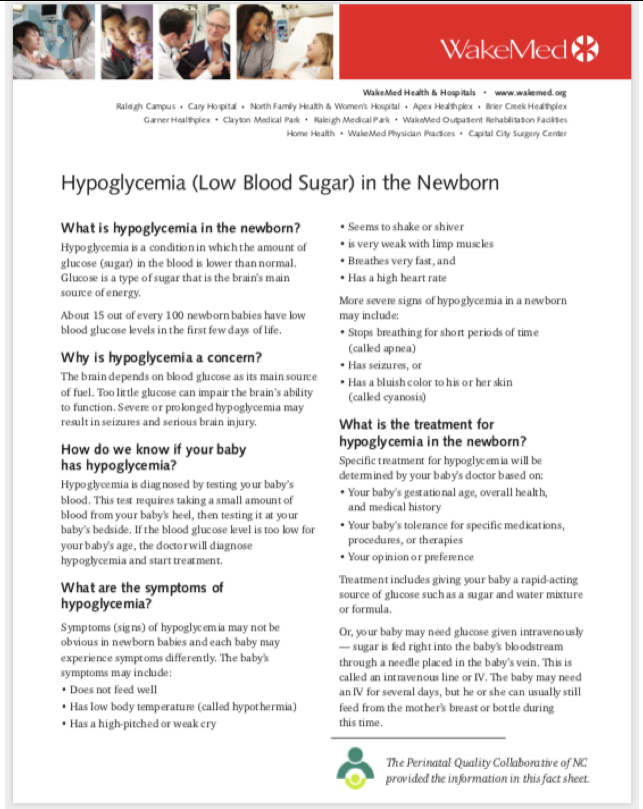
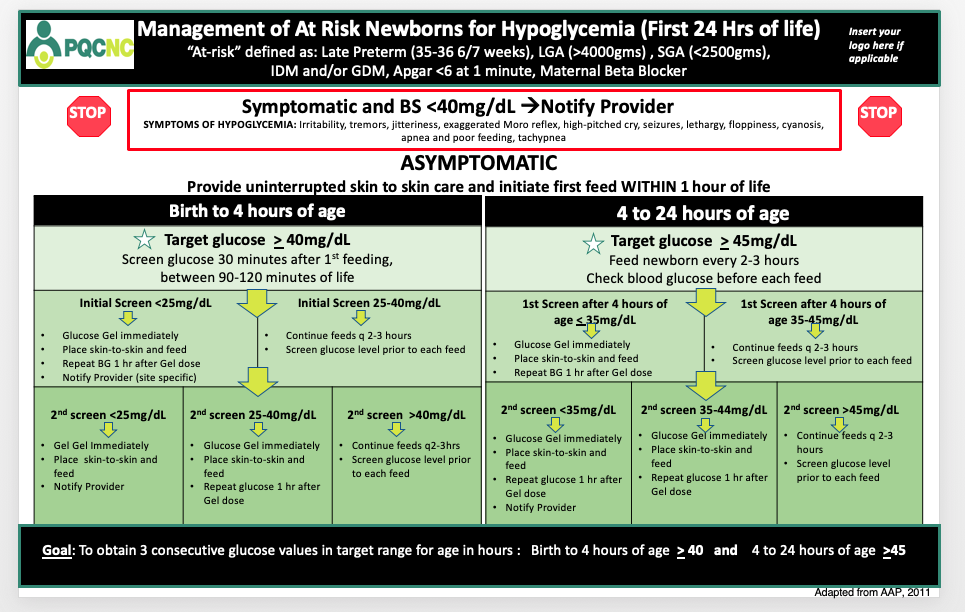
After several PDSA's and administrative approval and vetting, the UNC team utilized the PQCNC tracking tool resource to achieve success with implementing the North Carolina statewide hypoglycemia algorithm including the use of glucose gel. The tool serves several purposes from educating and empowering patients to partner in care, to providing a clear timeline of interventions and treatments. The tool tracks elements of care such as glucose levels, gel administration, and frequency of feedings as well as informs the parent why their newborn is at risk and being monitored. With careful planning, implementing, and adapting (including translating into Spanish), UNC has achieved great strides in ensuring staff compliance with the statewide hypoglycemia protocol as well as improving continuity of care between newborn nursery and NICU.